Adrian Wong is at The International Symposium on Intensive Care and Emergency Medicine, which is often affectionately known as “Brussels”. He has written a mega blog covering the talks he attended today – if you are there he would love you to come up to him, say hello and tell him what you think of his blog! JS
Opening plenary
Personalised Intensive Care Medicine (JL Vincent)
3Ps pyramid – population-based/broad definitions –> personalised. We need to move from population-based to precision medicine.
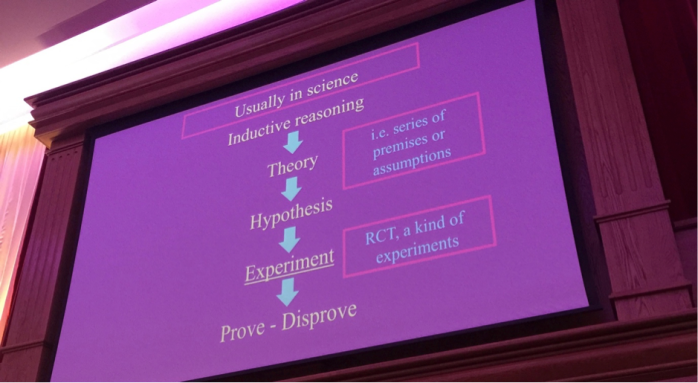
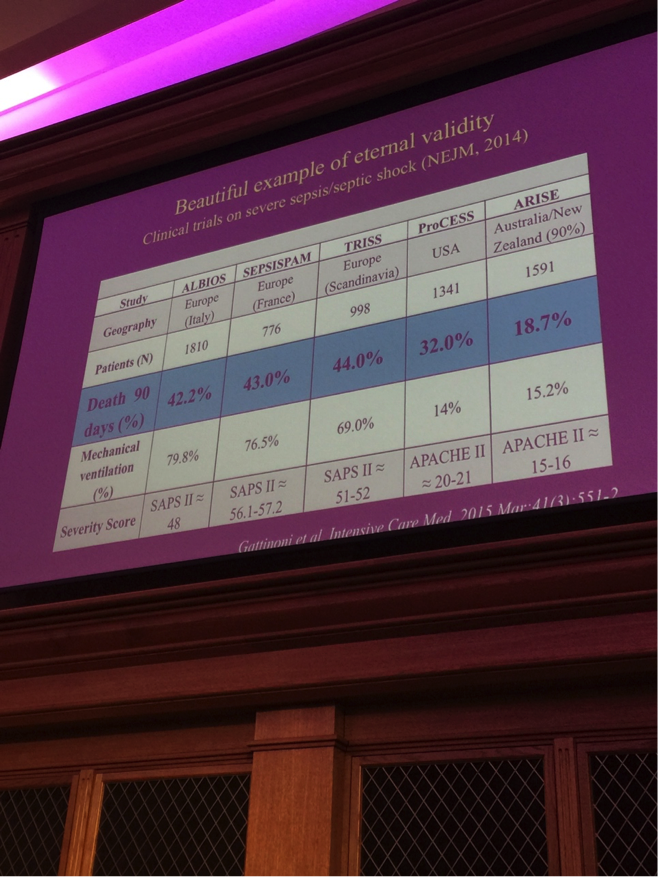
Failure of large RCTs in ICM can be in part be explained by the sheer heterogeneity of population being studied.
Medicine has always been personalised (Osler)
Genomics – does survival rely solely on the individual’s genetic makeup?
e.g. response to vasopressin is different in population
The host response to inflammation is variable
Biomarkers
ARTISAN study which looks at THROMBOMODULIN
Wong et al – Developing a clinically feasible personalized medicine approach to pediatric septic shock.
“SIRS is a hiccup in history”
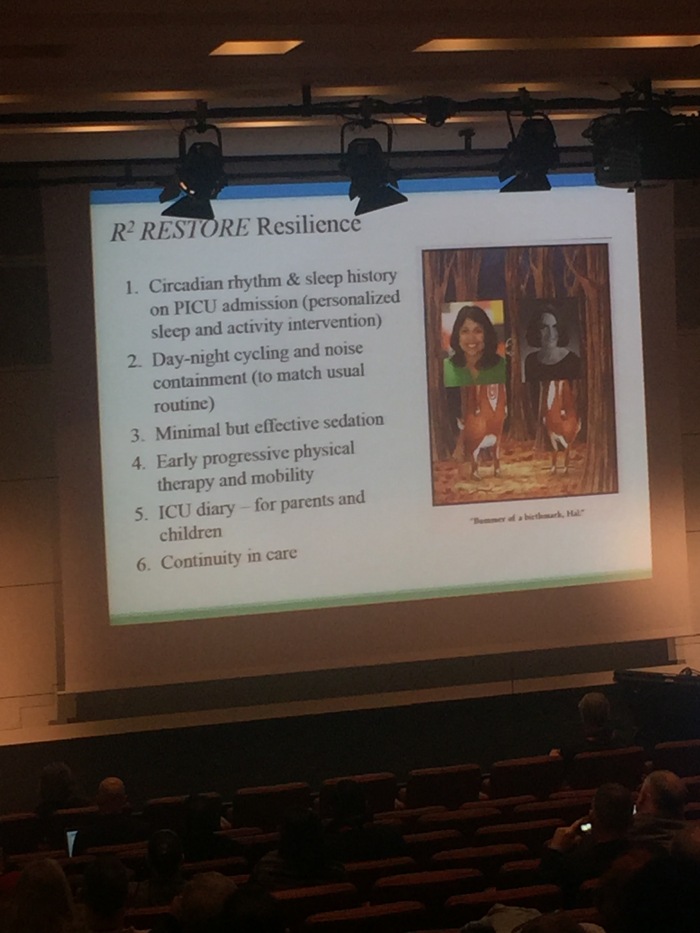
Report of round table meeting re: recovery after critical illness (Azoulay/Herridge)
3rd round table meeting – 2002 and 2009
2002 – Angus: Surviving Intensive Care
2009 – Griffiths and Hall: Exploring ICU-acquired weakness
Broached the idea of extending rehabilitation outside ICU but also focussed on the long-term effects on patients beyond ICU
Opportunities to improve care
- Critical care is a disease continuum
- Patient and family centred and engagement
- Sound biological plausibility
- Pts are heterogeneous
- Role of rehabilitation in changing outcome
Long term cognitive impairment after critical illness (BRAIN-ICU study)
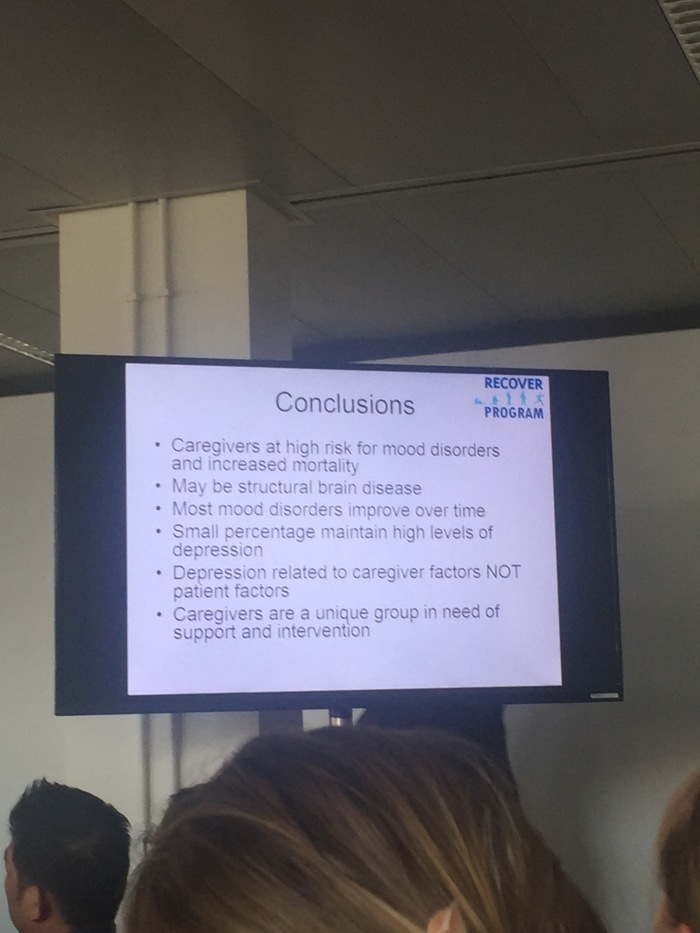
Depressive symptoms in patients and spouses are common
The Impact of High Versus Low Sedation Dosing Strategy on Cognitive Dysfunction in Survivors of Intensive Care Units: A Systematic Review and Meta-Analysis.
Early intensive care sedation predicts long-term mortality in ventilated critically ill patients.
The longer MV, the greater the weakness
NICE guidelines on rehabilitation after critical illness (2009)
Patient-centred outcomes/spiritual care – independent life, cognitive function, ability to work, absence of chronic pain, etc
These may not be the same as what the doctor is aiming for
Intensive care may need to integrate with palliative care
- Relieve distress
- Support person
- Manage uncertainties
- Elicit values
- Help caregivers
10 recommendations:
- Look outside the ICU and embrace continuum including pre-ICU trajectory/recovery/adaptation
- Patient and family engagement and personalised care
- Heterogeneity risk stratification
- Open the ICU doors
- Addressing pain
- Understand role, timing, indication and duration of rehabilitation
- Comprehensive understand of neuroendocrine derangements
- Role of long germ follow up
- Adoption of proven strategies from other clinical settings
- Development a comprehensive education agenda for all stakeholders
ICU-acquired infections (van der Poll)
Incidence, Risk Factors, and Attributable Mortality of Secondary Infections in the Intensive Care Unit After Admission for Sepsis
Host-response to sepsis: balance of pro- and anti-inflammatory response
Strategies = anti-inflammatory agents and immune stimulatory agents
Primary end-point – ICU-acquired infection (>48hrs after admission)
Patients who developed secondary infection where sicker (SOFA, APACHE2)
13.1% of patients admitted to ICU with sepsis will develop an ICU-AI (with attributable mortality of 10.9% by day 60)
15.1% of patients admitted to ICU with non-sepsis diagnosis will develop ICU-AI
Age isn’t a risk factor (with attributable mortality of 21.1% by day 60)
LOS with ICU-AI is significantly increased
DahLIA trial: Dexmedetomidine to lessen ICU agitation (Reade)
Effect of Dexmedetomidine Added to Standard Care on Ventilator-Free Time in Patients With Agitated Delirium
We don’t know how to treat delirium
Efficacy and safety of quetiapine in critically ill patients with delirium: a prospective, multicenter, randomized, double-blind, placebo-controlled pilot study.
Mechanism of dexmedetomodine – sedative a2-agonist (substantially less hypotentive than clonidine)
Inclusion – pts who remain intubated only because of their degree of agitation require such a high dose of sedative medication
Intervention dex 0.5ug/kg/hr (0-1.5) or placebo
Primary end-point: ventilator-free hours after extubation
74 patients randomised (96 target)
Fewer pts in dex group required additional sedative drugs
Dex group had significantly more ventilator-free hours: 144.8 vs 127.5
Nurses thought patient was ready for extubation quicker
Time to extubation faster
Dex patients had less time CAM-ICU positive
Adding dex to standard care is likely to be a cost-effective intervention
Early vs late parenteral nutrition in critically ill children (PEPaNIC) Van der Berghe
Early versus Late Parenteral Nutrition in Critically Ill Children
Critically ill patients unable to be fed by mouth
Cochrane collaborative (2009) Nutritional support in critically ill children
Nutritional practice in PICUs varies
- 70% start EN within 24-48hrs
- 50% start PN within 24-48hrs
- Adult trials question the benefit of early PN
This trial looked at early PN to supplement EN compared to EN alone
PN initiated within 24hrs after PICU admission
Both groups had early EN
End point – new infections and duration of PICU stay
1440 randomised
No difference in mortality (hint that early PN might be harmful)
Early PN associated with more infection
Duration of ICU stay increased by PN
Early PN increased MV days
Withholding PN for 1 week superior to early PN
Hypoxaemia following major surgery – NIVAS study (Jabir)
Effect of Noninvasive Ventilation on Tracheal Reintubation Among Patients With Hypoxemic Respiratory Failure Following Abdominal Surgery
Development and validation of a score or prediction of postop respiratory complications Brueckmann et al
A Trial of Intraoperative Low-Tidal-Volume Ventilation in Abdominal Surgery
Treatment of Acute Hypoxemic Nonhypercapnic Respiratory Insufficiency With Continuous Positive Airway Pressure Delivered by a Face Mask
This trial – primary outcome number of re-intubation within 7 days. Inclusion resp failure within 7 days of surgical procedure
300 pts randomised
NO HIGH-FLOW NASAL CANNULA. Only traditional NIV mask used
Re-intubation 46 (control) vs 33% (NIV)
NIV group had less lung infections within 30 days
NIV increased ventilator-free days
Post-extubation high-flow nasal cannula vs conventional oxygen therapy in low-risk pts
Effect of Postextubation High-Flow Nasal Cannula vs Conventional Oxygen Therapy on Reintubation in Low-Risk Patients
Would HFNO prevent reintubation in low risk pts within 72 hours
Low risk – <65, APACHE2<12, BMI<30, adequate secretion management, absence of heart failure, <1 co-morbidity, absence of airway patency problems
10347 screened; 527 randomised. Majority excluded as deemed high risk for intubation
HFNO had lower reintubation rate (4.9% vs 12.2%) – also less laryngeal oedema and stridor
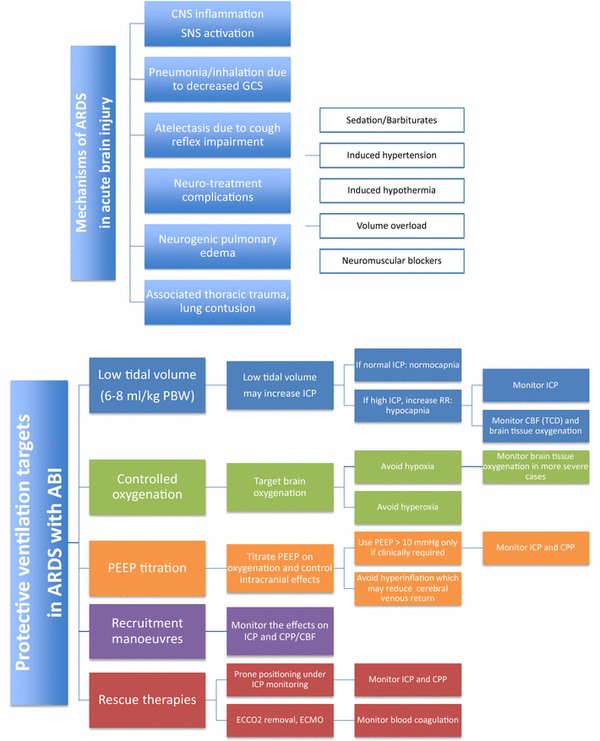
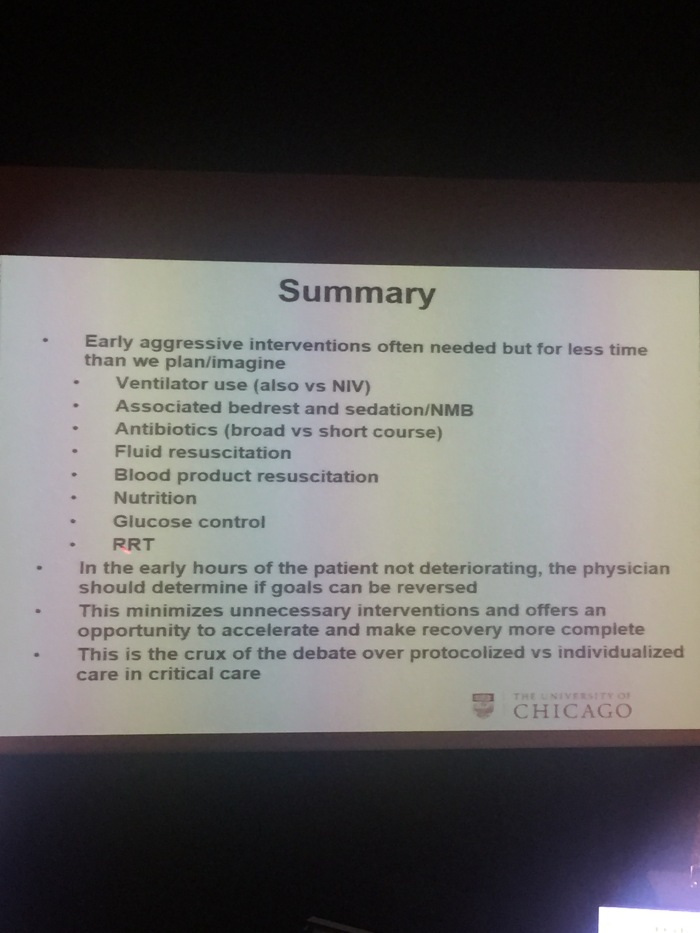
Individualised management of ARDS (L Brochard)
Max Harry Weil Memorial Lecture
ARDS initially described in Lancet 1967
LUNG-SAFE study
4499 pts with hypoxemic respiratory failure
3022 with ARDS
We don’t ventilate them very well – too much TV, PEEP variable etc.
ARDS – is not a single entity.
Comparisons of Berlin definition for ARDS with autopsy (Thille AW et al AJRCCM 2013)
Subphenotypes of ARDS (Calfee CS et al Lancet Resp Med 2014)
2 phenotypes identified – Phenotype 1 has better survival characteristics
Higher vs lower PEEP in ALI/ARDS Systematic Review (JAMA 2010)
PEEP induced lung volumes to predict alveolar recruitability (Dellamonica ICM)
Oxygenation response to PEEP predicts mortality in ARDS (Goligher EC et al)
ARDS management
The concept of the baby lung. Small lung does not mean stiff lung
Stress (pressure) and Strain (deformation)
Strain – increase in lung vol/FRC
Lung stress and strain during mechanical ventilation: any safe threshold?
Compliance = tidal volume/driving pressure
Driving Pressure and Survival in the Acute Respiratory Distress Syndrome
Conclusion
Reducing VILI is still the most important possibility to improve survival post ARDS. Individualised ventilation should be based on
- Recognising ARDS
- Assessing severity
- Individually titrating Vt (strain) and PEEP
SOSD Phases of fluid resuscitation
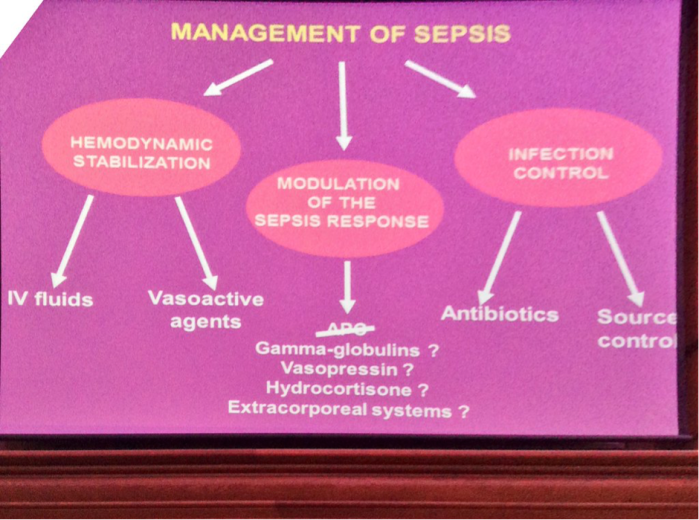
Circulatory Shock – JLV and De Backer
Four phases of intravenous fluid therapy: a conceptual model
Salvage (Shapiro)
- Fluid management in sepsis has changed considerably despite it being a time critical diagnosis
- Obtain a minimal acceptable BP
Perform lifesaving measures
(pic)
During salvage, LIBERAL FLUID RESUSCITATION – 30mls/kg??
ARISE, PROMISE, PROCESS
The Bottom Line – Fluid review section
Conclusion
- Approximately 4-5l
- IDENTIFY EARLY
- Antibiotics
- Ensure critical interventions
- Qns which fluid – anything you can swim in
- Qns diastolic dysfunction – becoming more important. BUT not in the salvage phase
- Qns what are your markers for success – multiple e.g. BP, HR, biochemistry. When you have a BP you can leave the bedside for a minute
Optimisation (De Backer)
- Provide adequate oxygen availability
- Optimise CO, SvO2, lactate
Why give fluids? Expect an increase in tissue perfusion
Delayed fluid is associated with greater activation of inflammation CCM 2012 40 2841
Improvement in microcirculation associated with improved organ function
Fluids and CO (Muller Anaesthesiology 2011) – not all improve CO
Why restrict fluids? Oedema deleterious – lung oedema and tissue oedema
A positive fluid balance is associated with a worse outcome in patients with acute renal failure
Sepsis in European intensive care units: results of the SOAP study.
The Adult Respiratory Distress Syndrome Cognitive Outcomes Study Long-Term Neuropsychological Function in Survivors of Acute Lung Injury
Fluid challenges in intensive care: the FENICE study A global inception cohort study
What DBD would do (pic)
Qns what markers? Lactate. Arterial Veno CO2 gradient
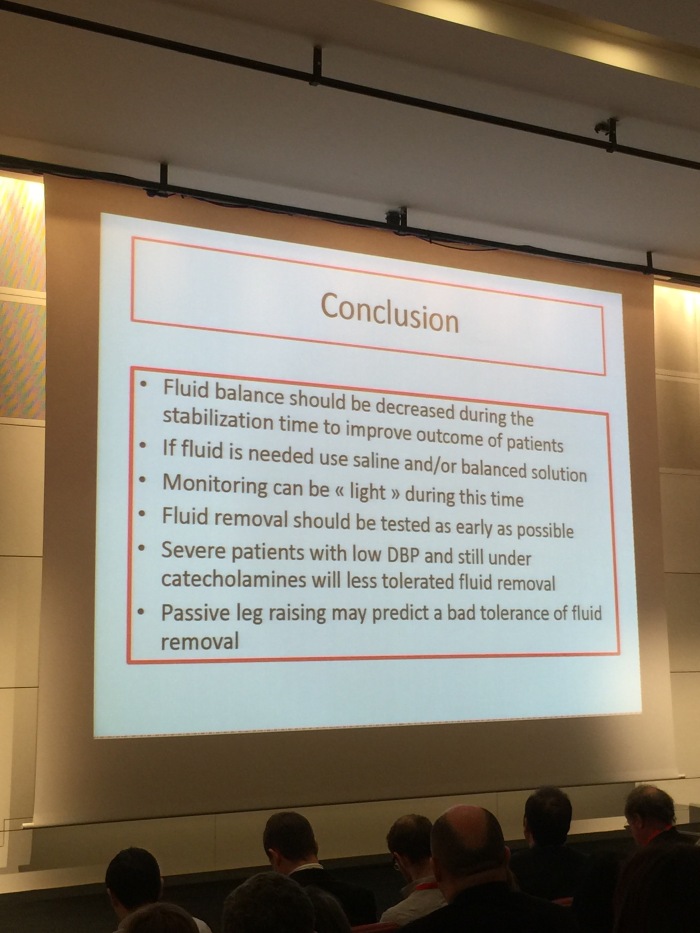
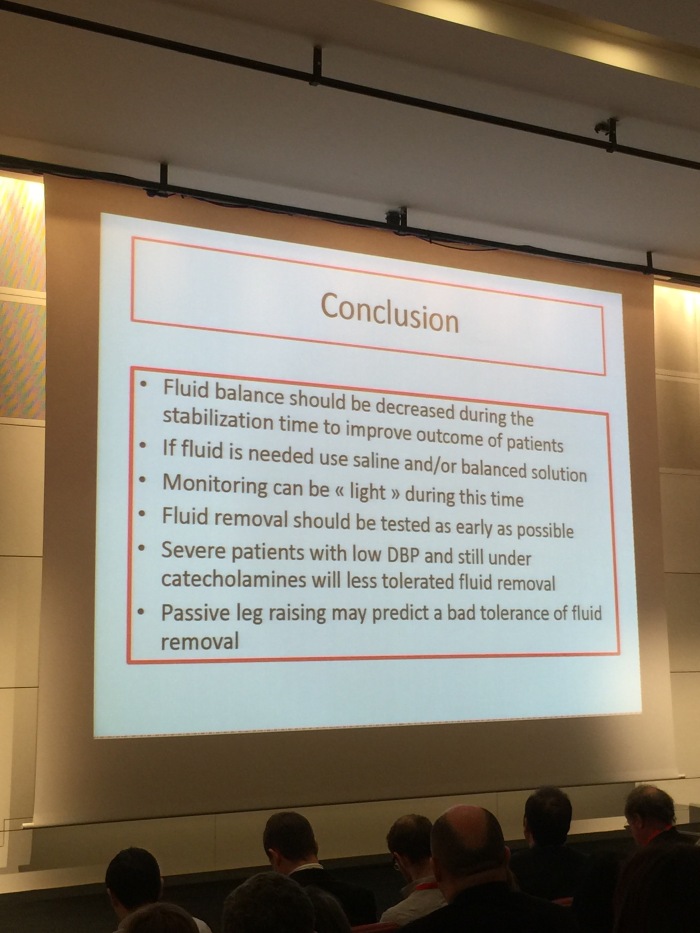
Stabilisation (Slama)
- Provide organ support
- Minimise complications
Aim for zero or negative balance during this phase
FINNAKI study – http://www.ncbi.nlm.nih.gov/pubmed/23075459
A positive fluid balance is an independent prognostic factor in patients with sepsis
Chloride – Association between intravenous chloride load during resuscitation and in-hospital mortality among patients with SIRS.
Meta-analysis of chloride – Meta-analysis of high- versus low-chloride content in perioperative and critical care fluid resuscitation.
RRT and diuretics to transition to de-escalation phase
De-escalation (Marshall)
- Wean for vasoactive drugs
- Achieve a negative fluid balance
Prefers the term de-resuscitation
How? Spontaneous, diuretics, RRT
Strategies – fluid restrict, initial resuscitation then restrict, active de-resuscitation
Who? >72 hrs in ICU and net fluid balance > 6l
Early resuscitation in sepsis
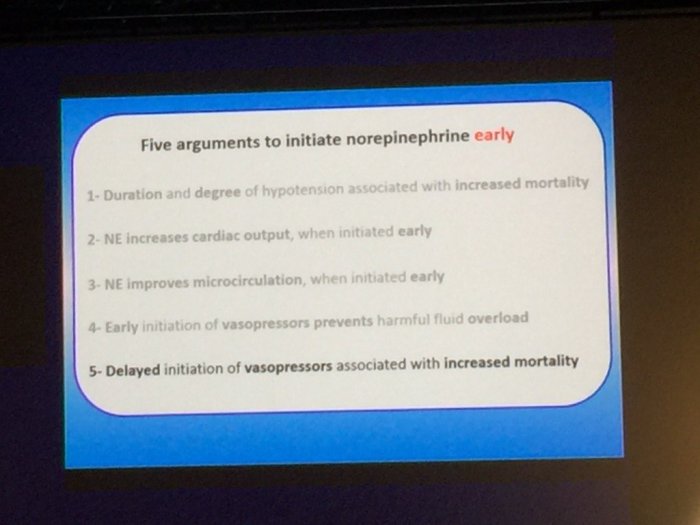
Arterial BP targets (JL Teboul)
Why do we use vasopressor?
When to initiate?
- Early. May not have completely be fluid resuscitate yet.
- Look at diastolic BP
Which MAP target in septic shock?
INDIVIDUALISED ASSESSMENT
Lots of oxygen (P Rademacher)
Altered oxygen extraction in illness and sepsis
Understanding the benefits and harms of oxygen therapy
Hyperoxia in experimental sepsis CCM 2009 37 2465
- In animals studies, hyperoxia is anti-inflammatory and improves hemodynamics/metabolism
- And does not cause ALI
Eur J Emerg Med 2014 31 233 Stojmeijer et al.
Hyper2S – hyperoxia and hypertonic saline (2*2 trial)
BUT trials stopped early due to worse outcome in both intervention groups
Results
- Hyperoxia group had better PaO2 (obviously)
- Hyperoxia group had better SOFA by D7
- BUT adverse events noted. Hyperoxia had more weakness, atelectasis
- Higher mortality in hyperoxia group at D28 and D90
Hyperoxia CANNOT be recommended in pts with septic shock
Should EGDT be abandoned (De Backer)
Varpula et al ICM 2005 31 1066
Rationale for EGDT – prevent development of tissue hypoperfusion achieving targets for MAP, SvO2 and CVP
Rivers – more fluids, RBC, Dobutamine and vasodilatory agents, sedation and mechanical ventilation. BUT criticism – single centre, potential confounders, few pts made the difference….
PROCESS, ARISE, PROMISE all didn’t show a difference
EGDT: do we have a definitive answer – De Backer and JLV
Difference with Rivers
High ScVO2 can mean anything!
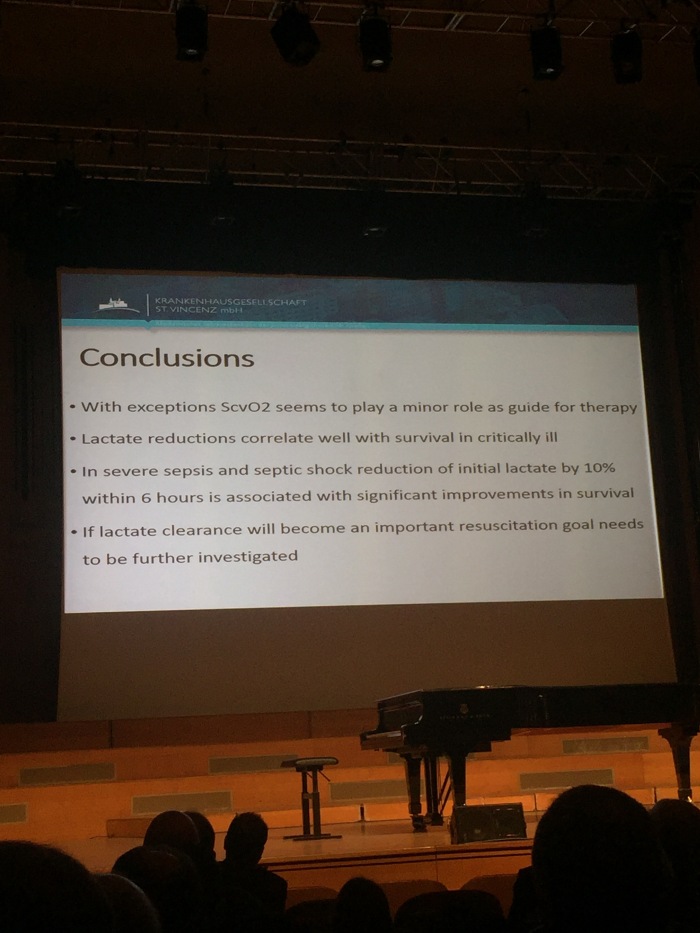
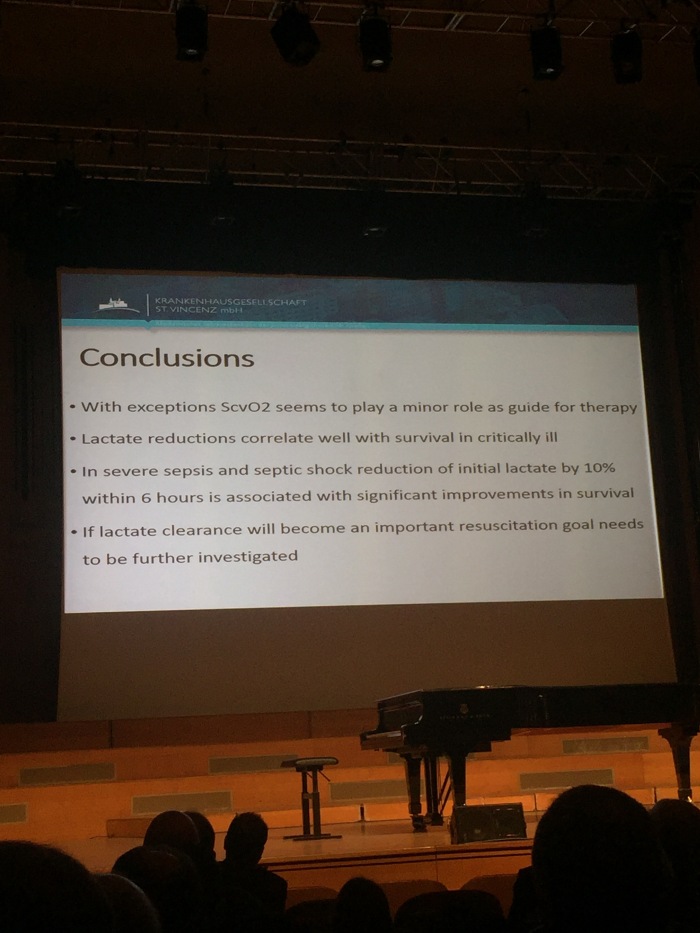
How useful are changes in lactate levels? (Fries)
EGDT what do we do now? Levy
Serum lactate as predictor of mortality in patients with infections (ICM 2007)
Serial blood lactate levels can predict the development of MOF following septic shcok (Bakker 1996 Am J Surg) – time with high lactate probably more important than the initial lactate
Lactate clearance
EMShockNet investigators – lactate clearance vs non-lactate clearance groups
Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial.
Lactate Clearance vs Central Venous Oxygen Saturation as Goals of Early Sepsis Therapy: A Randomized Clinical Trial
German Lactate in Severe Sepsis trial
HAEMODYNAMICS
How to interpret veno-arterial pCO2 (JLT)
Simplified Fick equation
High PCO2 difference is due to blood stagnation caused by low cardiac output state
6mmHg is the magic number
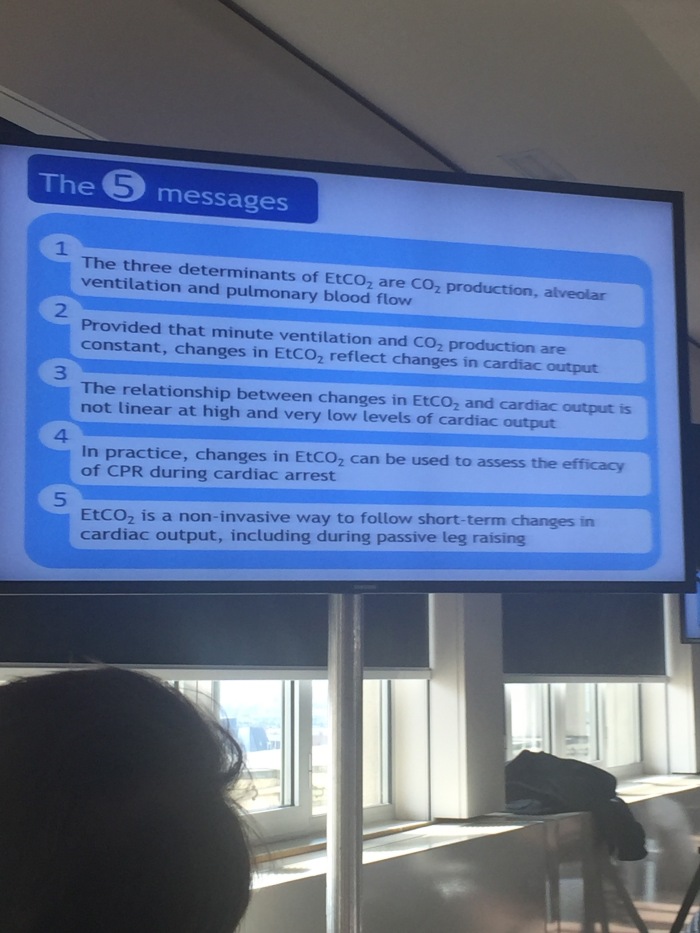
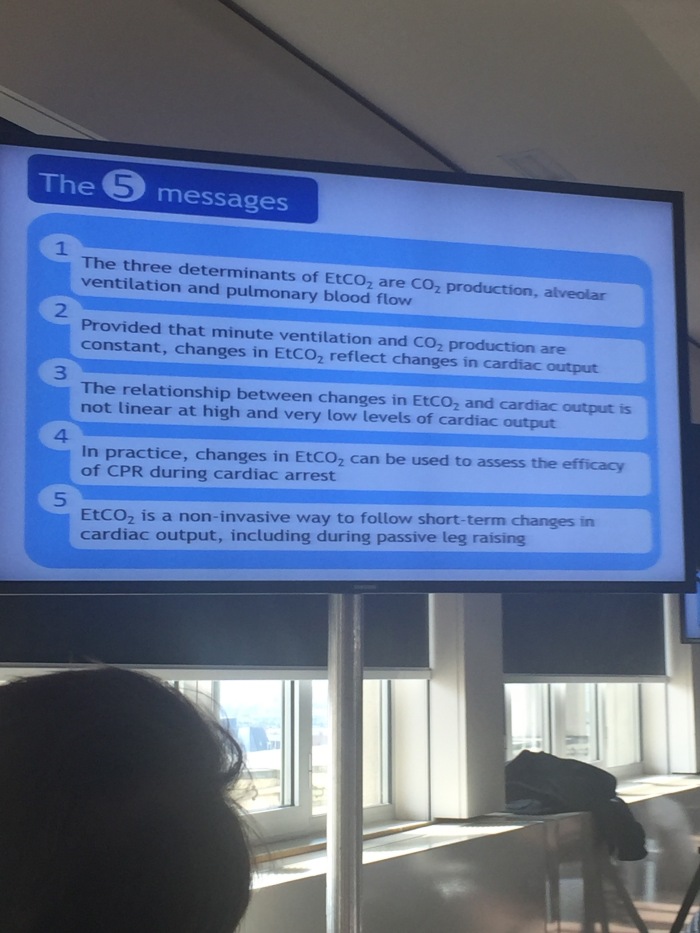
EtCO2 as a cardiac output monitor (Monnet)
Revision of physiology of etCO2
3 determinants of etCO2
- Alveolar ventilation
- Pulmonary blood flow
- CO2 production
Provided production of CO2 is constant, etCO2 can be used to reflect CO
End-tidal CO2 pressure determinants during hemorrhagic shock – http://www.ncbi.nlm.nih.gov/pubmed/11193267
Relationship between etCO2 and CO is not linear
Partial pressure of end-tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study – http://ccforum.biomedcentral.com/articles/10.1186/cc7009
etCO2 can be used with fluid balances
Haemodynamic monitoring
Why (Perel)
Haemodynamic instability in sepsis – http://www.ncbi.nlm.nih.gov/pubmed/14644922
Haemodynamic status of a critically ill patients is very complex
Clinical review: Update on hemodynamic monitoring – a consensus of 16 – http://ccforum.biomedcentral.com/articles/10.1186/cc10291
Getting the Full Diagnostic Picture in Intensive Care Medicine: A Plea for “Physiological Examination”
– http://www.atsjournals.org/doi/abs/10.1513/AnnalsATS.201509-571LE#.Vugk5BIrKRs
No evidence that any form of monitor improves outcome on the ICU
Perioperative cardiovascular monitoring of high-risk patients: a consensus of 12
http://ccforum.biomedcentral.com/articles/10.1186/s13054-015-0932-7
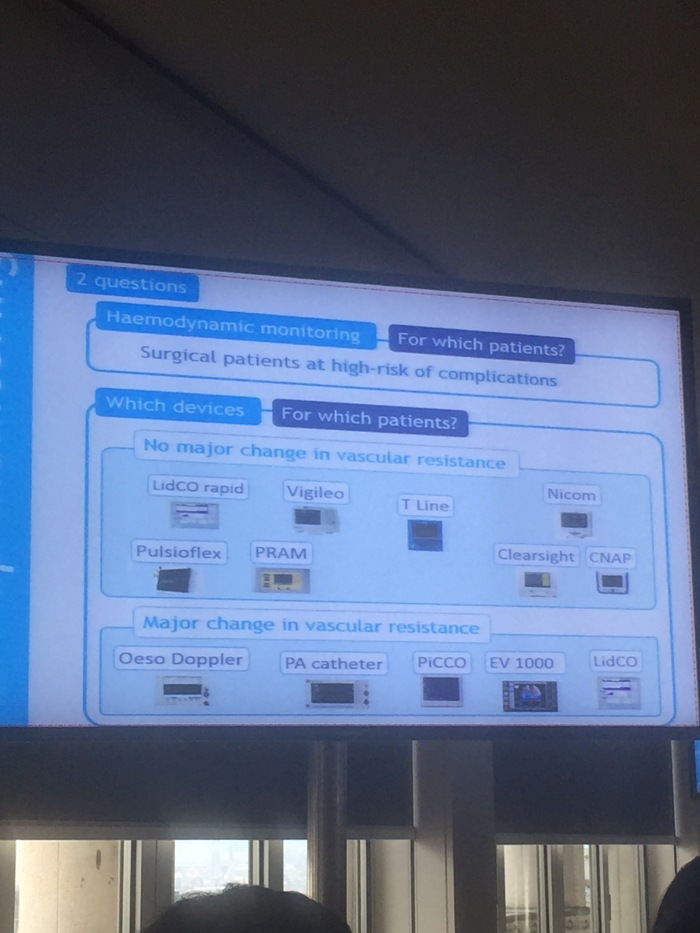
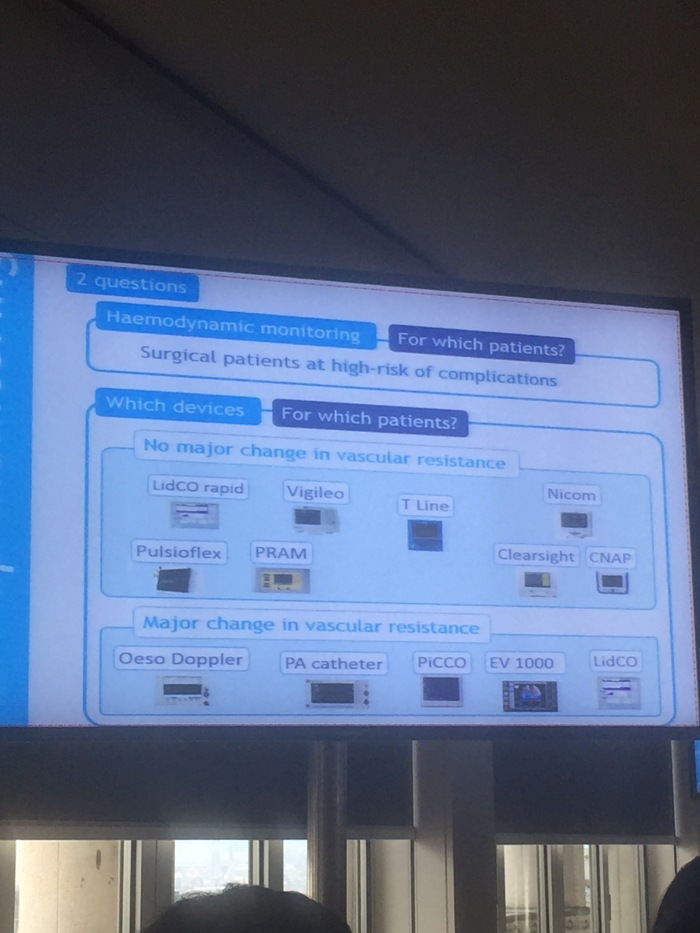
How (Biais)
- PAC
- Transpulmonary thermodilution
- Pulse pressure analysis
- Arterial line – calibrated vs non-calibrated
- Oesophageal Doppler
- Bio-reactance/bio-impedence
Conclusion
- Many device available
- Perfect device doesn’t exists
- Know limitations
- Will not improve outcome by itself
Who (Monnet)
Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet].
A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients
Choice of monitor in theatre depends on whether vascular resistance is going to be stable
Also see Robs trial summary:


















 (@Doctor_J_)
(@Doctor_J_)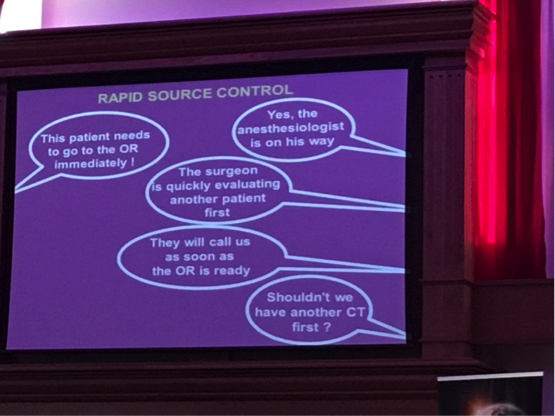 (@david_menzies)
(@david_menzies)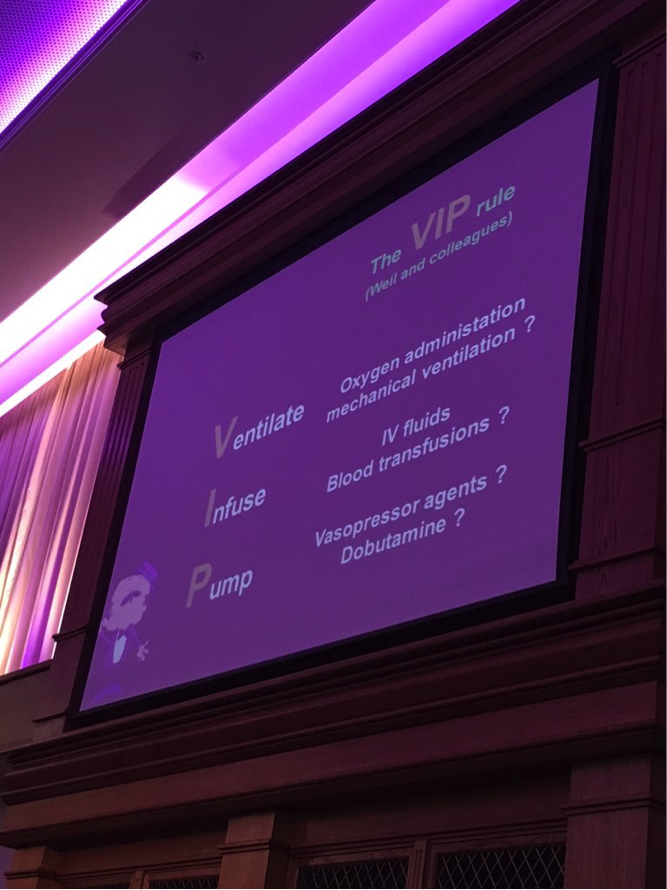 VIP – ventilate, infuse and pump
VIP – ventilate, infuse and pump
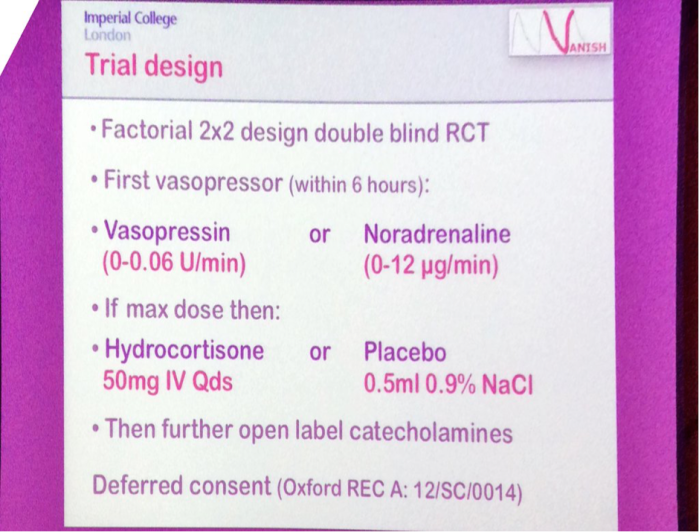
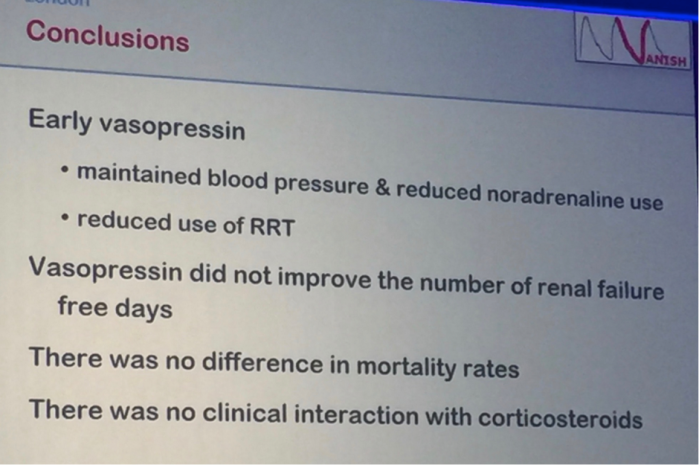 The role of vasopressin differs in health and shock/septic shock.
The role of vasopressin differs in health and shock/septic shock.